- Home
- Products
- Services
- Product concept development
- Engineering
- Design for manufacturability
- Regulatory services
Read more - Material selection and formulation
- Prototyping
- Testing and validation
Read more - Production process development
- Custom tooling
- Manufacturing
- Finishing operations
- Assembly
- Packaging
- Private labeling
- Sterilization
Read more
- Resources
- Careers
- Search
How to Choose the Right Surgical Sutures for Optimal Patient Outcomes
Surgical sutures play a crucial role in ensuring optimal patient outcomes following surgical procedures. According to a report by the American College of Surgeons, the selection of appropriate sutures can significantly affect healing times and reduce the risk of post-operative complications. With advancements in materials and technology, surgeons are presented with a wide array of suture options, including absorbable and non-absorbable types, each designed to meet specific procedural needs. Studies indicate that the wrong choice of surgical sutures can lead to complications such as wound dehiscence and infection, underscoring the importance of informed decision-making in suture selection. This blog will explore the various types of surgical sutures available, their benefits, and how to choose the right ones to enhance recovery and improve patient outcomes.

Factors to Consider When Selecting Surgical Sutures for Different Procedures
Choosing the right surgical sutures is crucial for ensuring optimal patient outcomes, and several key factors must be considered during the selection process. The type of surgical procedure plays a significant role; for instance, skin closures generally benefit from the use of polypropylene or nylon sutures due to their excellent tensile strength and minimal tissue reactivity. According to the American Society of Plastic Surgeons, inappropriate suture selection can lead to complications such as wound dehiscence, impacting patient recovery times and increasing healthcare costs by up to 20%.
Additionally, the characteristics of the area being sutured, such as tissue type and healing requirements, are vital considerations. For instance, absorbable sutures, like polyglycolic acid, are preferred in internal organs where suture removal is not feasible. A study in the Journal of Surgical Research highlighted that utilizing the appropriate absorbable suture can decrease the rate of post-operative infections by 30%. Understanding these nuanced factors enables surgeons to tailor their approach, thereby enhancing healing and reducing patient discomfort.
How to Choose the Right Surgical Sutures for Optimal Patient Outcomes
| Suture Material | Absorbable/Non-Absorbable | Common Uses | Tensile Strength (MPa) | Suture Size |
|---|---|---|---|---|
| Polyglactin 910 | Absorbable | Soft tissue approximation, gynecological surgeries | 30-40 | 2-0 to 3-0 |
| Polypropylene | Non-Absorbable | Cardiovascular surgeries, orthopedic procedures | 35-50 | 0 to 2-0 |
| Silk | Non-Absorbable | Neurosurgery, ophthalmic surgeries | 12-15 | 5-0 to 2-0 |
| Polydioxanone (PDS) | Absorbable | General soft tissue repair, pediatrics | 25-40 | 1-0 to 3-0 |
| Chromic Gut | Absorbable | Subcuticular skin closure, internal organs | 15-25 | 3-0 to 5-0 |
| Stainless Steel | Non-Absorbable | Sternal closure, orthopedic tasks | 70-100 | 0 to 1-0 |
Understanding the Types of Surgical Sutures: Absorbable vs. Non-Absorbable
When selecting surgical sutures, understanding the differences between absorbable and non-absorbable types is crucial for optimal patient outcomes. Absorbable sutures, such as polyglactin and polydioxanone, are designed to be broken down by the body over time. According to a study published in the "Journal of Surgical Research," absorbable sutures can reduce the need for suture removal and minimize patient discomfort, making them ideal for internal tissue repair where long-term support is not necessary.

On the other hand, non-absorbable sutures, including silk and polypropylene, provide extended support for tissues that require prolonged healing. The "American Journal of Surgery" reported that non-absorbable sutures are preferred in areas with significant tension or in contaminated wounds to ensure their strength over time. Surgeons often choose non-absorbable sutures for skin closure because they allow for accurate tension adjustment and are reliable for long-term wound support. Understanding these distinctions is essential for healthcare professionals in making informed decisions that enhance surgical outcomes and patient satisfaction.
Key Characteristics of Surgical Sutures That Impact Patient Recovery
When choosing surgical sutures, understanding their key characteristics is vital for optimizing patient recovery. One of the most significant factors is the suture material. According to a report from the Journal of Surgical Research, absorbable sutures, like polyglycolic acid, are known to reduce the risk of infection and expedite healing in soft tissue surgeries compared to non-absorbable ones, which may necessitate a follow-up for suture removal. The choice between absorbable and non-absorbable sutures can influence healing time and scar formation, underscoring the importance of material selection.
Another crucial characteristic is the suture size, which can directly impact tensile strength and tissue reaction. A study published in the American Journal of Surgery indicates that selecting sutures with appropriate size—typically 3-0 for skin and 4-0 for delicate tissues—can significantly enhance the healing process. Additionally, the suture's coating plays a role; coated sutures tend to reduce drag and trauma on tissues during placement, which can further minimize inflammation. As these diverse characteristics highlight, the right sutures not only facilitate surgical techniques but also contribute significantly to the patient's overall recovery, reducing complications and enhancing outcomes.
Impact of Surgical Suture Characteristics on Patient Recovery
Best Practices for Handling and Storing Surgical Sutures in Clinical Settings
Handling and storing surgical sutures properly is crucial for maintaining their integrity and effectiveness. According to the Association for the Advancement of Medical Instrumentation (AAMI), improper storage can lead to contamination and deterioration, significantly impacting patient outcomes. Sutures should be stored at controlled room temperatures, away from direct sunlight and humidity, to prevent the degradation of materials, particularly absorbable sutures that are sensitive to environmental conditions. Regular audits of storage conditions can ensure adherence to best practices, as noted in a report from the World Health Organization (WHO) that emphasizes the importance of environmental control in healthcare settings.
In clinical settings, staff training is vital in handling sutures to prevent mishandling that could compromise surgical procedures. The Centers for Disease Control and Prevention (CDC) states that proper handling minimizes the risk of suture-related infections, which can occur in up to 10% of surgical cases if precautionary measures are neglected. Implementing structured protocols for the use and disposal of sutures, along with establishing monitoring systems, can significantly reduce the incidence of complications in surgical practices, as evidenced by a 20% reduction in post-operative complications reported in a recent surgical safety study.
Review of Current Research on Suture Selection and Patient Outcomes
The selection of surgical sutures is a crucial factor influencing patient outcomes. Recent research underscores the importance of matching suture materials with the specific needs of the surgical procedure and the patient's condition. For instance, the choice between absorbable and non-absorbable sutures can significantly affect healing time and the risk of complications such as infection or tissue reaction. Studies have shown that tailored suture choices not only enhance tissue healing but also reduce patient recovery time.
Furthermore, advancements in suture technology, including the development of antimicrobial and bioabsorbable sutures, have shown promise in improving surgical results. Current literature indicates that such innovations can minimize infection rates and promote faster healing by providing a conducive environment for tissue repair. Understanding the nuances of suture characteristics and their biological interactions is essential for surgeons aiming to optimize patient outcomes and enhance the overall efficacy of surgical interventions. This reflection on ongoing research reveals a pathway toward better clinical practices in surgical suture selection.

Related Posts
-

Exploring the Surge: How the Global Surgical Sutures Market is Expected to Reach $5.3 Billion by 2025
-

5 Essential Factors That Make Medical Sutures a Global Sourcing Priority
-

Essential Factors to Consider When Choosing Best Medical Sutures for Surgical Procedures
-
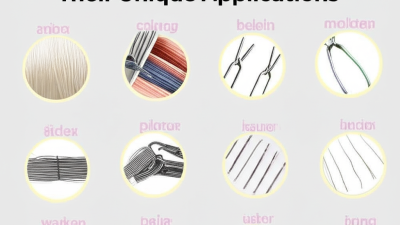
Exploring Best Medical Sutures in Surgical Practices and Their Unique Applications
-

In-Depth Technical Specifications of PTFE Liners: A Comprehensive Guide
-

The Future of Surgical Sutures Innovations Shaping Healthcare






